Mirena® is locally acting1
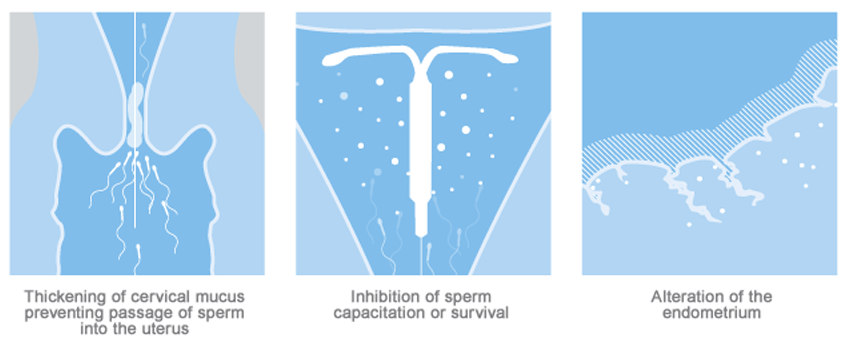
The local mechanism by which continuously released LNG contributes to the contraceptive effectiveness of Mirena has not been conclusively demonstrated.
Studies of Mirena and similar LNG IUS prototypes have suggested several mechanisms that prevent pregnancy:
- Mirena contains 52 mcg of levonorgestrel (LNG) released in vivo, at a rate of approximately 21 mcg/day after 24 days. This rate decreases progressively to approximately 11 mcg/day after 5 years and 7 mcg/day after 8 years1
- Estimated in vivo release rates for Mirena
Time Estimated in vivo release rate [μg/day] (rounded) 24 days after insertion 21 60 days after insertion 21 1 year after insertion 19 3 years after insertion 14 5 years after insertion 11 6 years after insertion 9 7 years after insertion 8 8 years after insertion 7 Average over 1st year 20 Average over 3 years 18 Average over 5 years 15 Average over 8 years 13 - After insertion of Mirena, LNG is detectable in serum/plasma after 1 hour. The maximum concentration is reached within 2 weeks after insertion and amounts to about 180 ng/L (CV 38%). In correspondence with the declining release rate, the geometric mean serum/plasma concentration of levonorgestrel declines continuously:
Estimated Total LNG Mean Plasma ConcentrationsTime after insertion Total LNG plasma concentrations [ng/L] (geometric CV%) 24 days 175 (37.6) 2 months 169 (37.1) 1 year 159 (37.4) 3 years 139 (37.8) 5 years 123 (38.2) 8 years 100 (39.9)
In the event of pregnancy
- If pregnancy should occur with Mirena in place, remove Mirena because leaving it in place may increase the risk of preterm labor and spontaneous abortion, including septic abortion. If a woman becomes pregnant with Mirena in place and if Mirena cannot be removed or the woman chooses not to have it removed, warn her that failure to remove Mirena increases the risk of miscarriage, sepsis, premature labor and premature delivery. Advise her of isolated reports of virilization of the female fetus following local exposure to LNG during pregnancy with an LNG IUS in place. Removal or manipulation may result in pregnancy loss.
- Evaluate women for ectopic pregnancy because the likelihood of a pregnancy being ectopic is increased with Mirena. Also consider the possibility of ectopic pregnancy in the case of lower abdominal pain, especially in association with missed menses or if an amenorrheic woman starts bleeding. Tell women about the signs of ectopic pregnancy and associated risks, including loss of fertility. Women with a history of ectopic pregnancy, tubal surgery, or pelvic infection carry a higher risk of ectopic pregnancy1
INDICATIONS FOR MIRENA®
Mirena® (levonorgestrel-releasing intrauterine system) 52 mg is indicated for prevention of pregnancy for up to 8 years; replace after the end of the eighth year. Mirena is indicated for the treatment of heavy menstrual bleeding for up to 5 years in women who choose to use intrauterine contraception as their method of contraception; replace after the end of the fifth year if continued treatment of heavy menstrual bleeding is needed.
IMPORTANT SAFETY INFORMATION ABOUT MIRENA
Who is not appropriate for Mirena
Use of Mirena is contraindicated in women with: known or suspected pregnancy and cannot be used for post-coital contraception; congenital or acquired uterine anomaly, including fibroids if they distort the uterine cavity; known or suspected breast cancer or other progestin-sensitive cancer, now or in the past; known or suspected uterine or cervical malignancy; liver disease, including tumors; untreated acute cervicitis or vaginitis, including lower genital tract infections (eg, bacterial vaginosis) until infection is controlled; postpartum endometritis or infected abortion in the past 3 months; unexplained uterine bleeding; current IUD; acute pelvic inflammatory disease (PID) or history of PID (except with later intrauterine pregnancy); conditions increasing susceptibility to pelvic infection; or hypersensitivity to any component of Mirena.
Clinical considerations for use and removal of Mirena
Use Mirena with caution after careful assessment in patients with coagulopathy or taking anticoagulants; migraine, focal migraine with asymmetrical visual loss, or other symptoms indicating transient cerebral ischemia; exceptionally severe headache; marked increase of blood pressure; or severe arterial disease such as stroke or myocardial infarction.
Consider removing the intrauterine system if these or the following arise during use: uterine or cervical malignancy or jaundice. If the threads are not visible or are significantly shortened they may have broken or retracted into the cervical canal or uterus. If Mirena is displaced (e.g., expelled or perforated the uterus), remove it.
Pregnancy related risks with Mirena
If pregnancy should occur with Mirena in place, remove the intrauterine system because leaving it in place may increase the risk of spontaneous abortion and preterm labor. Advise her of isolated reports of virilization of the female fetus following local exposure to LNG during pregnancy with an LNG IUS in place. Removal or manipulation may result in pregnancy loss. Evaluate women for ectopic pregnancy because the likelihood of a pregnancy being ectopic is increased with Mirena. Also consider the possibility of ectopic pregnancy in the case of lower abdominal pain, especially in association with missed menses or if an amenorrheic woman starts bleeding. Tell women about the signs of ectopic pregnancy and associated risks, including loss of fertility. Women with a history of ectopic pregnancy, tubal surgery, or pelvic infection carry a higher risk of ectopic pregnancy.
Educate her about PID
Mirena is contraindicated in the presence of known or suspected PID or in women with a history of PID unless there has been a subsequent intrauterine pregnancy. IUDs have been associated with an increased risk of PID, most likely due to organisms being introduced into the uterus during insertion. Promptly examine users with complaints of lower abdominal pain or pelvic pain, odorous discharge, unexplained bleeding, fever, genital lesions or sores. Inform women about the possibility of PID and that PID can cause tubal damage leading to ectopic pregnancy or infertility, or infrequently can necessitate hysterectomy, or cause death. PID is often associated with sexually transmitted infections (STIs); Mirena does not protect against STIs, including HIV. PID may be asymptomatic but still result in tubal damage and its sequelae.
In Mirena clinical trials, upper genital infections, including PID, occurred more frequently within the first year. In a clinical trial with other IUDs and a clinical trial with an IUD similar to Mirena, the highest rate occurred within the first month after insertion.
Expect changes in bleeding patterns with Mirena
Spotting and irregular or heavy bleeding may occur during the first 3 to 6 months. Periods may become shorter and/or lighter thereafter. Cycles may remain irregular, become infrequent, or even cease. Consider pregnancy if menstruation does not occur within 6 weeks of the onset of previous menstruation.
If a significant change in bleeding develops during prolonged use take appropriate diagnostic measures to rule out endometrial pathology.
Be aware of other serious complications and most common adverse reactions
Some serious complications with IUDs like Mirena are sepsis, perforation and expulsion. Severe infection, or sepsis, including Group A streptococcal sepsis (GAS) have been reported following insertion of Mirena. Aseptic technique during insertion of Mirena is essential in order to minimize serious infections, such as GAS.
Perforation (total or partial, including penetration/embedment of Mirena in the uterine wall or cervix) may occur, most often during insertion, although the perforation may not be detected until sometime later. The risk of uterine perforation is increased in women who have recently given birth, and in women who are breastfeeding at the time of insertion. In a large US retrospective, postmarketing safety study of IUDs, the risk of uterine perforation was highest when insertion occurred within ≤6 weeks postpartum, and also higher with breastfeeding at the time of insertion. The risk of perforation may be increased if Mirena is inserted when the uterus is fixed, retroverted or not completely involuted. If perforation occurs, locate and remove Mirena. Surgery may be required. Delayed detection or removal of Mirena in case of perforation may result in migration outside the uterine cavity, adhesions, peritonitis, intestinal perforations, intestinal obstruction, abscesses, and erosion of adjacent viscera. In addition, perforation may reduce contraceptive efficacy and result in pregnancy.
Partial or complete expulsion of Mirena may occur resulting in the loss of contraceptive protection. The risk of expulsion is increased with insertions immediately after delivery and appears to be increased with insertion after second-trimester abortion based on limited data. In the same postmarketing study, the risk of expulsion was lower with breastfeeding status. Remove a partially expelled Mirena. If expulsion has occurred, a new Mirena can be inserted any time the provider can be reasonably certain the woman is not pregnant.
Ovarian cysts may occur and are generally asymptomatic, but may be accompanied by pelvic pain or dyspareunia. Evaluate persistent enlarged ovarian cysts.
The most common adverse reactions reported in ≥5% of users were alterations of menstrual bleeding patterns [including unscheduled uterine bleeding (31.9%), decreased uterine bleeding (23.4%), increased scheduled uterine bleeding (11.9%), and female genital tract bleeding (3.5%)], abdominal/pelvic pain (22.6%), amenorrhea (18.4%), headache/migraine (16.3%), genital discharge (14.9%), vulvovaginitis (10.5%), breast pain (8.5%), back pain (7.9%), benign ovarian cyst and associated complications (7.5%), acne (6.8%), dysmenorrhea (6.4%), and depression/depressive mood (6.4%).
A separate study with 362 women who have used Mirena for more than 5 years showed a consistent adverse reaction profile in Years 6 through 8. By the end of Year 8 of use, amenorrhea and infrequent bleeding are experienced by 34% and 26% of users, respectively; irregular bleeding occurs in 10%, frequent bleeding in 3%, and prolonged bleeding in 3% of users. In this study, 9% of women reported the adverse event of weight gain, it is unknown if the weight gain was caused by Mirena.
Teach patients to recognize and immediately report signs or symptoms of the aforementioned conditions. Evaluate patients 4 to 6 weeks after insertion of Mirena and then yearly or more often if clinically indicated.
For important information about Mirena, please see the accompanying Full Prescribing Information.
Reference: 1. Mirena [prescribing information]. Whippany, NJ: Bayer HealthCare Pharmaceuticals; 2021.